Published on 12.05.2021
Mickaël Ménager, an Inserm researcher and director of a research lab and of the Single-Cell@Imagine LabTech, explains how this technology will make it possible to improve knowledge and management of genetic diseases.
How will the single cell analysis LabTech you are deploying change the understanding of genetic diseases?
Mickaël Ménager: From one cell to another in a sick patient, we can encounter different disturbances. Until now, when we looked at the genes expression of a sick person, we had, as it were, access to an average transcriptomic profile, not taking into account the individual characteristics of each cell. But sometimes it is there, in a cell that has so far gone unnoticed by us, that we find the answer to our questions about the origin of the disease, why it does not respond to this or that treatment, why the disease does not evolve in the same way as in another patient... It is by taking into account all the cells, despite, and above all because of the considerable amount of data that this represents, that we will be able to take a new step in the understanding of genetic diseases.
In concrete terms, how does it work?
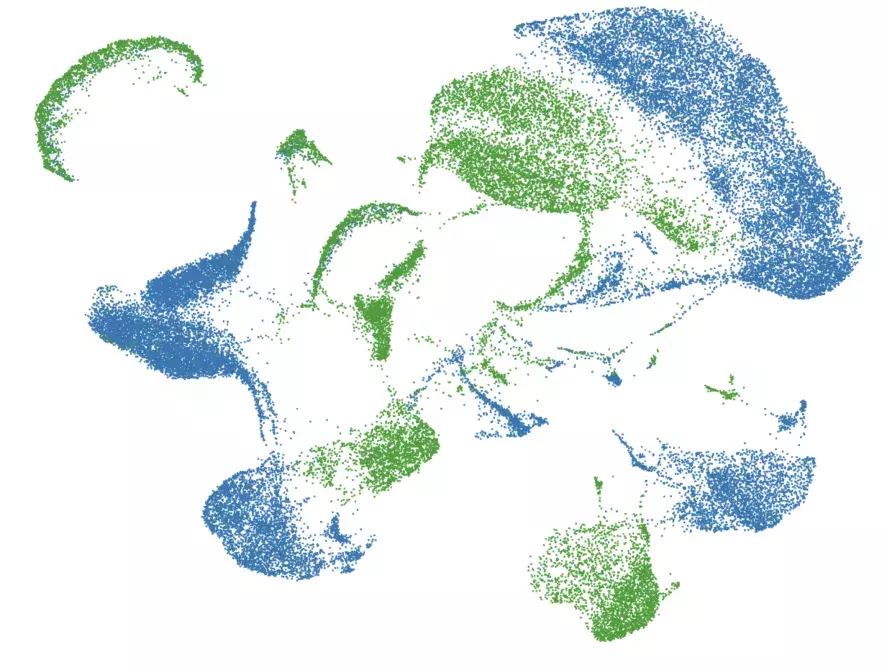
MM: Thanks to microchannels and microfluidics, each cell is isolated in an individual droplet in which chemical reactions take place to recover the RNA corresponding to the genes that are most expressed. Then, the use of sequencing, bioinformatics and the learning machine makes it possible to analyze all this data and generate an ID of the individual cell state.
It is then possible to compare the ID of different patients with or without the same pathology. We will thus most certainly be able to discover common points between certain diseases that were previously considered to be totally different. And a treatment for cholesterol could, for example, treat a group of patients suffering from a genetic autoimmune disease.
Ultimately, this technology is likely to become a therapeutic decision aid by facilitating the choice of the treatment best suited to the patient's cellular state, targeted at populations of abnormal cells and having proven its effectiveness on similar profiles, but also its adaptation over time according to the response of the disease. It is also expected to revolutionize prognosis since, on the basis of these cell profiles, the evolution of diseases could be known and therefore better anticipated.
Can we talk about personalized medicine in this case?
MM: The Single-Cell analysis does indeed appear to be one of the pillars for the development of a truly personalized medicine that takes into account as much data as possible about the individual and his or her illness.
With single-cell analysis, we are changing scale: it is as if until now we had been observing the human body with a zoom X10 microscope and now we have a zoom x1000. In one go, we can now analyze the expression of thousands of genes on more than 10,000 cells per individual.
What I hope is that in a few years' time, in addition to the clinical signs, when a patient arrives for a consultation, the doctor will be able to establish his or her cellular ID. All of this data will then be taken into account to identify the patient's disease, its evolutionary risk and the best treatment to offer.
Do you already have convincing results?
MM: As far as I'm concerned, in collaboration with Frédéric Rieux-Laucat's Lab, I'm studying more specifically diseases where the immune system overreacts and the organism starts to react as if it were invaded by a virus, even when this is not the case. Several parts of the body are then destroyed, including healthy cells, which causes autoinflammatory pathologies.
We are still in "proof of concept" phases, but we have very promising results for certain immune deficiencies. Our objective is to analyse the 2000 most expressed genes, cell by cell, in young patients in order to understand how the disease makes its nest in the organism and progressively destroys it.
Over the last few weeks, with Frédéric Rieux-Laucat's Lab, we have been heavily monopolized on research into severe forms of COVID-19 - which is very similar to the pathologies we are used to studying with a runaway immune system - and children with forms resembling Kawasaki disease. Thanks to the American company 10X Genomics, a partner in the COVID-19 project, we were quickly able to install a new Chromium in an L3 containment laboratory for the study of blood cells from COVID-19 patients.
The idea is therefore to go and look at the expression of immunity genes in patients with moderate COVID-19, then to monitor their evolution and to carry out a new analysis in the 5% who will develop an Acute Respiratory Distress Syndrome. We thus hope to determine a predictive signature of patients at risk of developing a severe form, but also to identify the immune pathways involved to counteract them.
Is this platform accessible to other researchers?
The technologies available in this LabTech, namely 2 Chromium Controller devices to generate cell encapsulations and catalogues of the most expressed genes, a Chromium Connect controller to produce catalogues of single cell transcripts in an automated manner and a PCR device are accessible to all Imagine laboratories and more widely to all researchers in the Ile-de-France region.
This LabTech has received €0.6 million in support as part of the SESAME PIA Filières PIA call for projects in 2019.
It has also been selected by 10x Genomics to be among the first 45 members of the Visium translational clinical research network, giving us access to a global community of researchers working on this innovative approach.
Analyses of gene expression at the Single-Cell level to better understand why children develop Kawasaki-like multi-inflammatory syndromes after SARS-CoV2 infection.
What a surprise in spring when an unexpected number of children infected with SARS-COV2 were hospitalized in the intensive care unit for Kawasaki-like forms, an inflammatory disease. Nearly half of them then rapidly developed acute myocarditis, which is an inflammation of the myocardium, the main muscle of the heart. At Institut Imagine, Frédéric Rieux-Laucat and Mickaël Ménager's Lab, in collaboration with Julie Toubiana and Darragh Duffy's teams at Institut Pasteur, as well as numerous clinicians, therefore wanted to find out more about the mechanisms at the origin of this inflammatory disease. Thanks to the Single-Cell, they were able to detect the expression of differentially expressed genes in 17 young patients who had developed myocarditis more than a month after infection with SARS-Cov-2, compared with other children who were infected but had not developed this severe form. A molecular signature seems to be emerging," says Mickaël Ménager. Now we need to confirm it and, above all, to validate it in the clinic to see if it would actually identify children who will develop myocarditis after an SARS-CoV2 infection. "This lead would open the way to better care for these patients and therefore to better treatment.