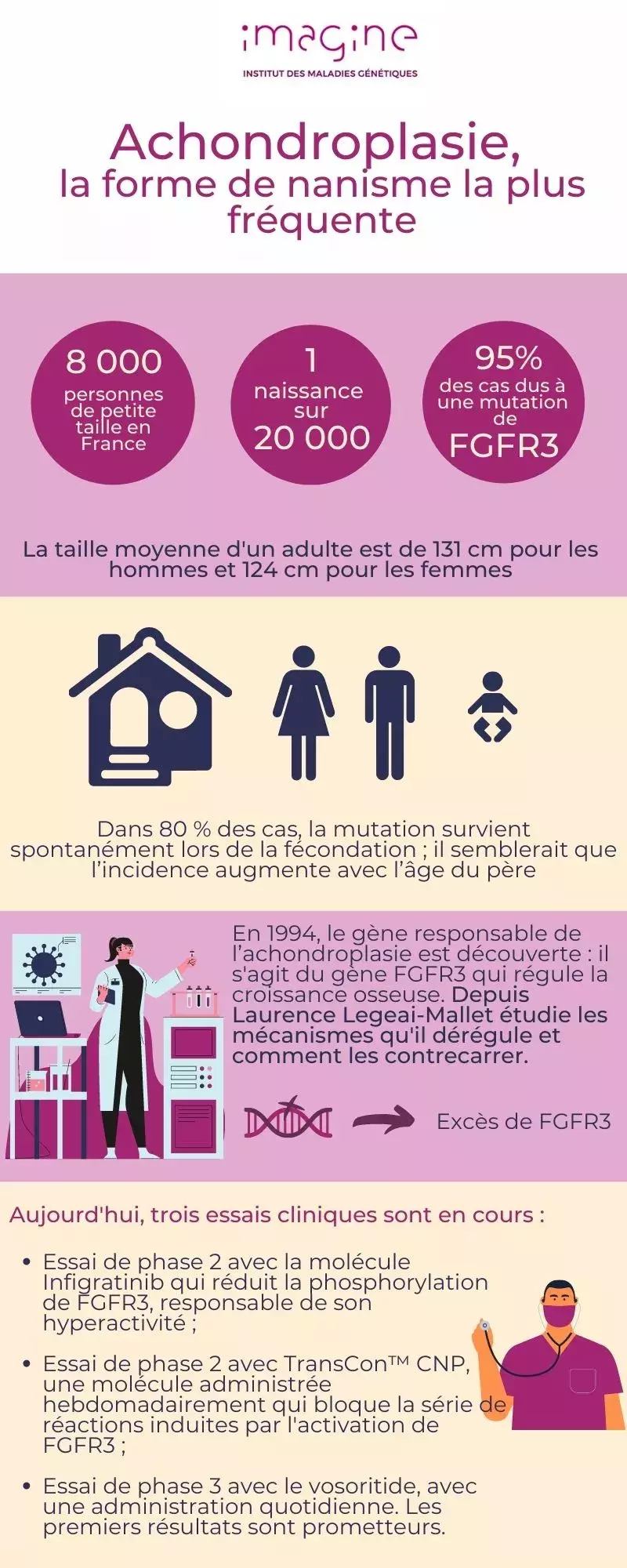
Achondroplasia is the most common form of dwarfism. It affects about one in 20,000 births. The main feature of this disease is a much smaller than average height, associated with a shortening of the limbs: the average height of an adult is 131 cm for men and 124 cm for women. Due to a defect in bone growth, people with achondroplasia also have a large disproportion between a medium sized trunk, very short legs and arms, a lordosis and a larger than average skull (macrocephaly).
Of the gene responsible...
It was in 1994 that Laurence Legeai-Mallet co-discovered the gene responsible for achondroplasia, the FGFR3 gene. Since then, the researcher joined Institut Imagine at its creation with the "Molecular and physiopathological bases of osteochondrodysplasias" (Inserm/Université de Paris) laboratory which she directs after having helped to create it with Valérie Cormier-Daire. Since then, she has continued to explore the mechanisms deregulated by the alteration of this gene and to develop cellular and animal models to test different molecules to counteract its deleterious effects.
One of the surprising facts is that in 99% of cases, patients carry the same FGFR3 mutation: it is a "false sense" mutation that causes a single "letter" in the part of the genome containing the information needed to produce the FGFR3 protein to change. In 80% of cases, the mutation occurs spontaneously during fertilization; it appears that the incidence increases with the age of the father. This leads to excess production of the FGFR3 protein, which alters ossification, the mechanism that transforms cartilage tissue into bone, gradually from childhood to puberty.
"Cartilage forms a large part of the skeleton during early development. In achondroplasia, the problem lies not only in the formation of cartilage, but in its formation into bone, especially in the long bones of the arms and legs and the vertebrae," she explains.
... to deregulated mechanisms ...
Bone growth is controled by the FGFR3 protein present on the surface of cartilage cells, the chondrocytes, but also of early forms of bone cells, the osteoblasts. Through its mutation in achondroplase patients, FGFR3 is permanently activated, disturbing the balance between proliferation and differentiation of these cells in the growth plate, the site of bone progression. As a result, bone elongation is reduced.
During infancy and childhood, bone growth occurs gradually, with an active phase before puberty. Bone elongation is essentially determined by the activity of the various growth plates and the formation of ossification centers, both of which are affected in achondroplasia as a result of the FGFR3 mutation.
Diagnosis: clinical and radiological
In 80% of cases, it is a de novo mutation and therefore did not exist in the parents. Prenatal ultrasound can identify common features of achondroplasia such as shortened limbs, short skull base and narrow chest. These features usually do not appear until 26 weeks of gestation. However, only the FGFR3 gene analysis certifies the diagnosis in the prenatal period. If the diagnosis could not be established beforehand, it is made at birth following clinical and radiological analyses.
In addition to short stature and short legs and arms, achondroplasia is accompanied by other medical problems such as pain, sleep apnea, recurrent ear infections, spinal cord compression that can lead to paralysis, in addition to daily difficulties and psychosocial disorders.
...to the therapeutic molecule...
Until very recently, treatment options for people with achondroplasia were limited to heavy and painful surgical modalities to lengthen long bones.
Knowledge of the mutated gene and its consequences has led to the development of new therapeutic options. Laurence Legeai-Mallet and her team have been largely involved in deciphering the mechanisms associated with the hyperactivity of the FGFR3 protein. This protein is one of the four signaling tyrosine kinase receptors (FGFRs) that interact with proteins that control fibroblast growth factor (FGF) signaling in mammals. Defects in the FGF pathway are implicated both in developmental disorders, such as dwarfism, but also in a wide range of cancers, including bladder, myeloma, cervical, prostate and testicular cancers as well as in benign tumors (nevi, acanthosis nigricans...).
In addition to deciphering the mechanisms deregulated by the FGFR3 mutation, Laurence Legeai-Mallet and her team have set out to find molecules capable of counteracting the hyperactivity of FGFR3, particularly among those used in oncology. As a result, in 2016, they published results showing that NVP-BGJ398 was a possible candidate. At the time, this molecule, under the name Infigratinib, was undergoing a Phase 2 clinical trial at Novartis to treat patients with bile duct cancer, a therapeutic avenue that has since been abandoned.
“NVP-BGJ398 reduces the phosphorylation of FGFR3, responsible for its hyperactivity, said Legeai-Mallet, and corrects abnormal femoral growth in our animal models of the disease. In addition, we demonstrated that a low dose of NVP-BGJ398, injected subcutaneously, was able to penetrate the growth plate in these same models and modify its organization. »
...and to clinical trials
Today this molecule (Infigratinib) is undergoing a clinical trial by QED Therapeutics. On July 15, 2020, the first administration of the molecule was performed in a young patient in Melbourne, Australia in a Phase 2 clinical trial coordinated internationally by Ravi Savarirayan of the Murdoch Children's Research Institute in Melbourne, Australia.
The positive results of another clinical trial also piloted by Ravi Savarirayan have also just been revealed: they concern vosoritide, a molecule developed by BioMarin, based on preclinical studies conducted by Laurence Legeai-Mallet. The phase 3 study - the phase just before commercialization - shows that children with acondroplasia treated with this molecule gained an average of 1.57 cm in one year compared to other untreated children. No major side effects were noted, but the treatment requires a daily injection.